Knee pain is a common issue that affects people of all ages. The knee is a hinge-like structure providing our body with flexibility, support, and a wide range of motion for our legs.1 This weight-bearing joint bears significant stress as we perform our usual routines, and it serves a powerful role in gait (walking patterns) and locomotion (the ability to walk forward).
The knee is the largest joint in the body and comprises a series of bones, ligaments, cartilage, and tendons. The knee is a team player who works with the other parts of the leg to function! The knee’s proper movement allows us to go for a jog, climb stairs, sit for long periods, and even allows our favorite basketball player to pivot on the court as they line up for that perfect shot at the basketball hoop.
But how does the knee work? What does it do in the body, and is it susceptible to injury? What does it mean if someone has knee pain? Is knee pain treatable? To answer these questions, it is important to understand the structures inside the knee and how they move and protect the joint!

Understanding the anatomy
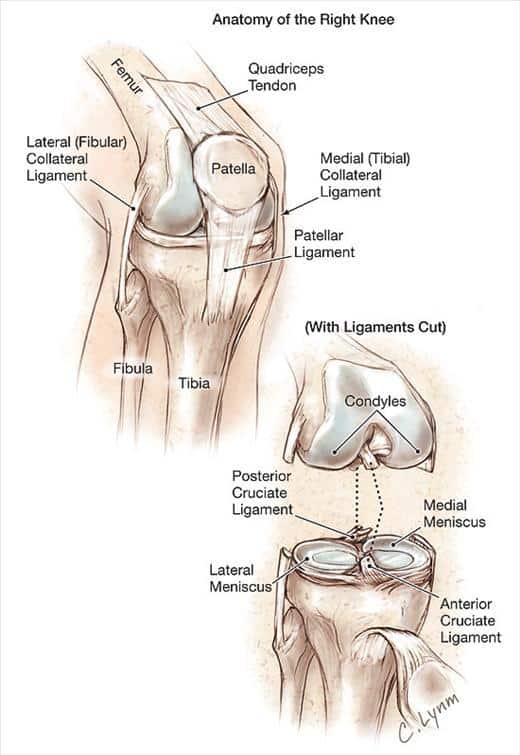
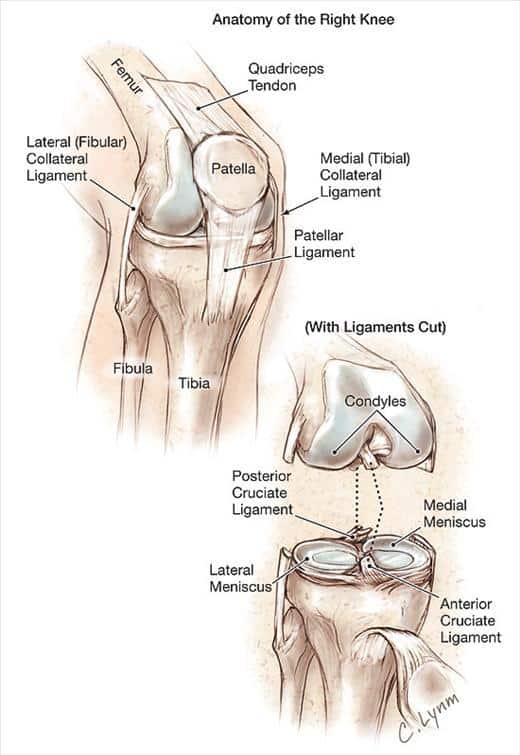
Your knee joint is a junction of several bones: the kneecap (patella), the shin bone (tibia), and the thigh bone (femur).
Between the bones is a rubbery, C-shaped cartilage called the meniscus that cushions and protect the bones.2 The meniscus absorbs internal and external forces on the joint. This function lets us jump on trampolines, walk downstairs, and apply our body weight onto the knee without pain. Athletes are prone to injuring the meniscus when too much force is applied to the joint; you may have watched your favorite football player roll into a tackle and injure their meniscus during a game, resulting in several weeks being missed as the player heals.
Another type of cartilage lines the bones of the knee where they connect. This slippery cartilage, called articular cartilage,2, allows for smooth movements of the bones around the knee joint. Articular cartilage protects bone surfaces from rubbing and grating on each other. This soft tissue structure prevents wearing down or degeneration of bony surfaces. You may have heard the phrase “bone on bone” to describe joints; articular cartilage helps prevent this!
Within and surrounding the knee are several important, rope-like ligaments connecting the bones. Several muscles from the pelvis, butt, and hip regions also connect to the knee. Several small-but-powerful muscles are specific to the knee, too. Lastly, tough, rubbery cords of tissue called tendons connect the muscles to the bones.
Is the knee prone to injury?
The knee is prone to pain due to wear and stress on the joint. Normal aging, repetitive activity, traumas, and sudden movement can create a knee injury. This is due to the knee’s role in lower extremity (leg) movements and the combination of bone surfaces together.
Not all knee injuries or knee conditions feel the same, either. Some types of knee pain are described as dull and achy, sharp, burning, pulling, tight, or sore. Knee pain can also feel like a deep aching in the joint or right on top of the skin.
Some injuries that occur to the knee are:
- Arthritis
- Fracture
- Tendinitis
- Bursitis
- Torn knee cartilage
- Dislocated kneecap
- Sprained ligaments
- Muscle tears
- Patellofemoral pain syndrome
- And more
Problems in the knee can result from trauma or a medical condition.3 A knee injury can also exist without pain! When the knee is not working properly, inflammation and other symptoms can occur. You may have symptoms of a knee condition such as clicking, popping, and locking up or giving out of the knee. You may notice your knee has decreased overall movement, or specific movements cause discomfort.
Knee pain may not involve the entire knee, either. Some individuals report having knee pain on one side of the knee. Knee pain can occur in the front, on the back, on the inner or outer sides, or deep within the knee joint. Sometimes pain can prevent proper movement and functioning, such as weight-bearing, on the knee.4 The location of the pain is an important characteristic regarding knee pain treatment.4,5,6
Who is at risk for developing knee pain? Several risk factors increase the likelihood of developing a knee injury. These include increasing age,4,5 being overweight, certain diseases like gout or autoimmune conditions, previous history of injury, lack of exercise, and more.3
Additionally, if the lower back or pelvis is misaligned or off balance, this can cause you to put more of your body weight on one side versus the other. Over time the added weight and stress placed on that knee joint can lead to increased risk of injury, sprains and strains and cause the cartilage to wear down faster than normal.
When do I see a doctor?
You should make an appointment with a musculoskeletal specialist if you have:
- Difficulty or loss of ability to walk comfortably on the affected side
- Knee pain that occurs while resting or at night
- Injury that causes knee deformity
- Swelling of the joint or the calf area
- Knee pain that persists longer than several days
- Difficulty or loss of ability to bend the knee
- Signs of infection or inflammation including fever, warmth, swelling, or erythema (redness)
- Any other unusual symptoms prompting immediate medical attention
How is knee pain treated?
Knee pain and knee injuries are best diagnosed with a proper evaluation and assessment. A doctor of chiropractic is a musculoskeletal specialist and the right person to assess the most common knee conditions. If the doctor needs more information, he or she may include imaging such as x-rays to visualize bones and joint spaces or an MRI to visualize soft tissues like ligaments and muscles for possible injury. Many knee diagnoses are based on medical history and physical examination alone!
Treatment options will depend on the severity, duration, and frequency of the pain and the cause of the condition. Some people seek treatment for knee conditions even without dysfunction to improve movement and quality of life.7,8<

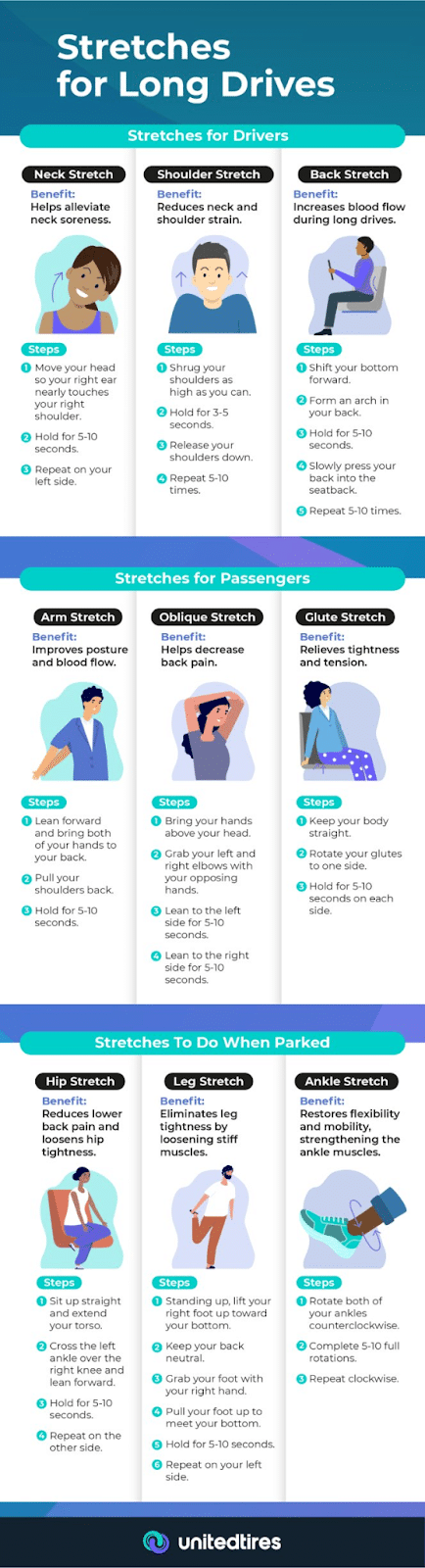
Conservative care can be very effective in treating different forms of knee pain. Thankfully, there are many options available to a person. Conservative care may include specific stretches for muscles and tendons of the knee, injection of a steroid or lubrication into the knee, joint mobilization, specific exercises to strengthen the surrounding muscles and tendons, hands-on soft tissue work into the muscles and fascia, changes in exercise routine or modifications at work or home, home exercise, and stretching programs, and more. <

Suppose your knee pain is due to an injury. In that case, your condition may be co-managed by your doctor with another healthcare professional such as a primary care doctor, orthopedist, or physical therapist.<
If you’re experiencing knee pain, it may go away on its own in a few days. However, if the pain does not go away or it keeps returning, then it’s time to call Back 2 Health Physical Medicine and make an appointment for a proper evaluation. <
References<
1. Zeller, J.M., Lynm, C., and Glass, R.M. (2007). Knee Pain. JAMA. 2007;297(15):1740.
2. Netter, Frank H. Atlas of Human Anatomy. 1906-1991. Philadelphia, PA: Saunders/Elsevier, 2014.
3. “Causes and tips for coping with chronic knee pain.” (2018). Medical News Today. Retrieved March 2021 from https://www.medicalnewstoday.com/articles/311308.
4. Farrokhi, S., Chen, Y. F., Piva, S. R., Fitzgerald, G. K., Jeong, J. H., & Kwoh, C. K. (2016). The Influence of Knee Pain Location on Symptoms, Functional Status, and Knee-related Quality of Life in Older Adults With Chronic Knee Pain: Data From the Osteoarthritis Initiative. The Clinical Journal of Pain, 32(6), 463–470.
5. Foroughi, N., Smith, R.M., Lange, A.K., Baker, M.K., Fiatarone Singh, M.A., Vanwanseele, B. (2010). Dynamic alignment and its association with knee adduction moment in medial knee osteoarthritis. Knee. Jun;17(3):210-6.
6. Farrokhi, S., Piva, S.R., Gil, A.B., Oddis, C.V., Brooks, M.M., Fitzgerald, G.K. (2013). Association of severity of coexisting patellofemoral disease with increased impairments and functional limitations in patients with knee osteoarthritis. Arthritis Care Res (Hoboken). Apr;65(4):544-51.
7. Rubin, B.R. (2005). Management of Osteoarthritic Knee Pain. J Am Osteopath Assoc;105:S23–S28.
8. Frese, T., et al. (2013). Knee Pain as the Reason for Encounter in General Practice. International Scholarly Research Notices Hindawi. Retrieved March 2021 from https://www.hindawi.com/journals/isrn/2013/930825.<